Peripheral arterial disease
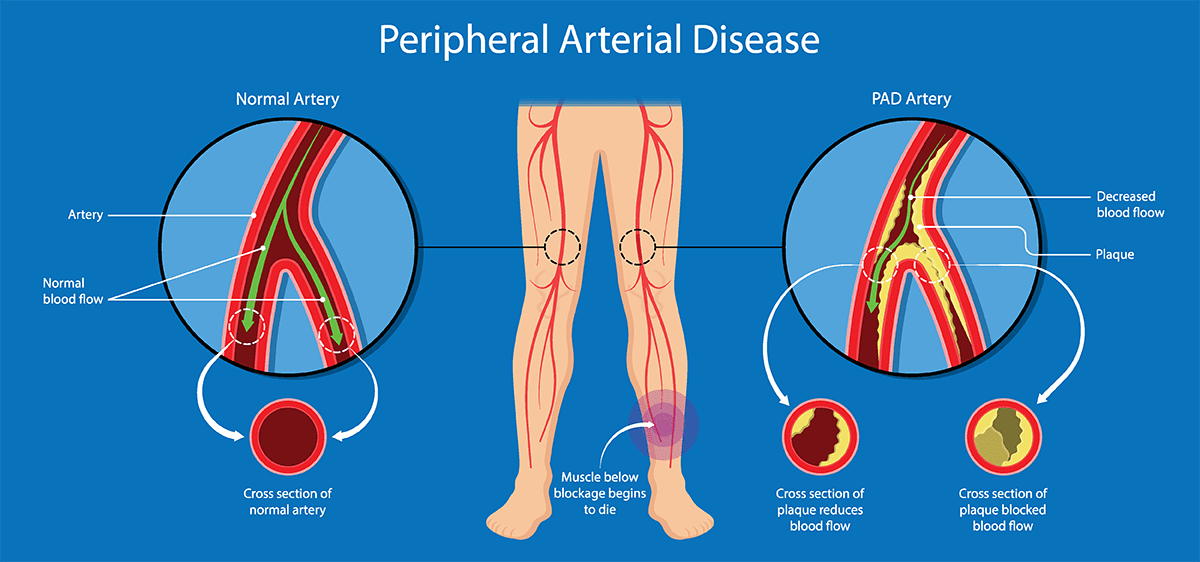
Peripheral arterial disease is a common condition, in which a build-up of fatty deposits in the arteries restricts the blood supply to leg muscles.
It's also commonly known as peripheral vascular disease.
Symptoms
Many people with peripheral vascular disease have no symptoms. However, some develop a painful ache in their legs when they walk, which usually disappears after a few minutes' rest. The correct medical term for this is "intermittent claudication". The pain can range from mild to severe.
Both legs are often affected at the same time, although the pain may be worse in one leg. Other symptoms can include:
Hair loss on legs and feet
Numbness or weakness in the legs
Brittle, slow-growing toenails
Ulcers (open sores) on feet and legs, which don't heal
Changing skin colour on legs, such as turning pale or blue
Shiny skin
In men, erectile dysfunction
The muscles in the legs shrinking (wasting)
The symptoms of PAD often develop slowly, over time. If your symptoms develop quickly, or get suddenly worse, it could be a sign of a serious problem requiring immediate treatment.
When to see a Dr
You should see Dr if you experience recurring leg pain when exercising.
Many people mistakenly think this is just part of growing older, but there's no reason why an otherwise healthy person should experience leg pain.
Peripheral vascular disease is usually diagnosed through a physical examination by a Dr, and by comparing the blood pressure in the arm and the ankle.
A difference between the two may indicate peripheral vascular disease and is called the ankle brachial pressure index.
Causes of peripheral arterial disease
Peripheral vascular disease is a form of cardiovascular disease meaning that it affects the blood vessels.
It's usually caused by a build-up of fatty deposits in the walls of the leg arteries. The fatty deposits, called atheroma, are made up of cholesterol and other waste substances.
The build-up of atheroma on the walls of the arteries makes the arteries narrower and restricts blood flow to the legs. This process is called atherosclerosis.
There are certain things that can increase the chances of developing peripheral vascular disease and other forms of cardio vascular disease, including:
Smoking – The the most significant risk factor
Type 1 and 2 diabetes
High blood pressure
High cholesterol
The risk of developing peripheral vascular disease also increases with age, and men tend to develop the condition more often than women.
Treatment
Peripheral vascular disease is largely treated through lifestyle changes and medication.
Exercising regularly and stopping smoking, are the main lifestyle changes that can ease the symptoms peripheral vascular disease and reduce the chances of the condition getting worse. It's also important to:
Eat a healthy diet
Lose weight, if overweight or obese
Moderate the consumption of alcohol
The underlying causes should also be treated, including high blood pressure, high cholesterol, and diabetes the legs.
With treatment, most people's symptoms remain relatively stable and some people may experience an improvement in their pain.
If treatment is unsuccessful or if the appropriate lifestyle changes can’t be made, there's a risk of potentially serious complications.
Complications
Peripheral vascular disease isn't immediately life-threatening, but the process of atherosclerosis that causes it can lead to serious and potentially fatal problems.
The blockages in the arteries in the legs can also affect other areas of your body, such as the arteries supplying the heart and brain.
This means that having peripheral vascular disease makes it more likely to develop another form of cardiovascular disease such as:
Coronary heart disease
Stroke
Heart attack
Angina
Critical limb ischaemia
If the blood flow to the legs becomes severely restricted, critical limb ischaemia can develop. This is an extremely serious complication that can be challenging to treat.
Symptoms include:
Severe burning pain in the legs and feet that continues even when resting
The skin turning pale, shiny, smooth and dry
Wounds and ulcers (open sores) on feet and legs that don't heal
Loss of muscle mass in the legs
The skin on toes or lower limbs becoming cold and numb, turning red and then black, and/or beginning to swell and produce foul-smelling pus, causing severe pain
If you think you're developing symptoms of Critical limb ischaemia, contact your Dr immediately.
If this isn't possible, go to an emergency department at the local hospital.
An angioplasty or bypass graft is usually recommended for critical limb ischaemia, although these may not always be successful or possible. In a few cases, an amputation below the knee may be required.
For more information or to book an appointment
call the Family Medical Centre on
+34 966 865 072, emailing us at
info@albirfamilymedicalcentre.com or on Facebook www.facebook.com/albirfamilymedicalcentre